Pressure Care – Why It’s Important
The most common parts of the body to get a pressure sore are the sacrum, heels and the ischial tuberosities, which combined account for around 70% of pressure sores developed in adults [1].
We must ensure that we carefully consider pressure care when providing any seating for our clients to minimise the risk of our client developing a pressure injury.
When thinking about pressure care we must consider the factors that make our clients more at risk of developing pressure sores. Factors such as poor nutrition, incontinence, poor sensation or reduced mobility increase the risk of our client developing a pressure sore. Clients who have a current pressure sore or who have had one in the past are also more at risk of significant pressure injury.
A detailed assessment of our client’s risk of developing pressure sores should always be completed and careful consideration given to the type of seating to be provided if our clients have any of these risk factors. We must also remember that seating will often be one part of a larger care or support plan for our client’s, but nonetheless a very important factor.
Pressure:
When the body is in a seated position there will be significant pressure being placed around bony prominences such as the sacrum and ischial tuberosities. If our client is unable to redistribute their body weight themselves they will be at increased risk of a pressure injury. NICE guidelines advise that adults deemed at high risk of pressure injury should change their position regularly, and at least every four hours[1]. We need to ensure that if our client is going to be seated in the same position for a long duration that a suitable plan is developed to assist them to change position regularly as well as considering pressure redistribution cushions.
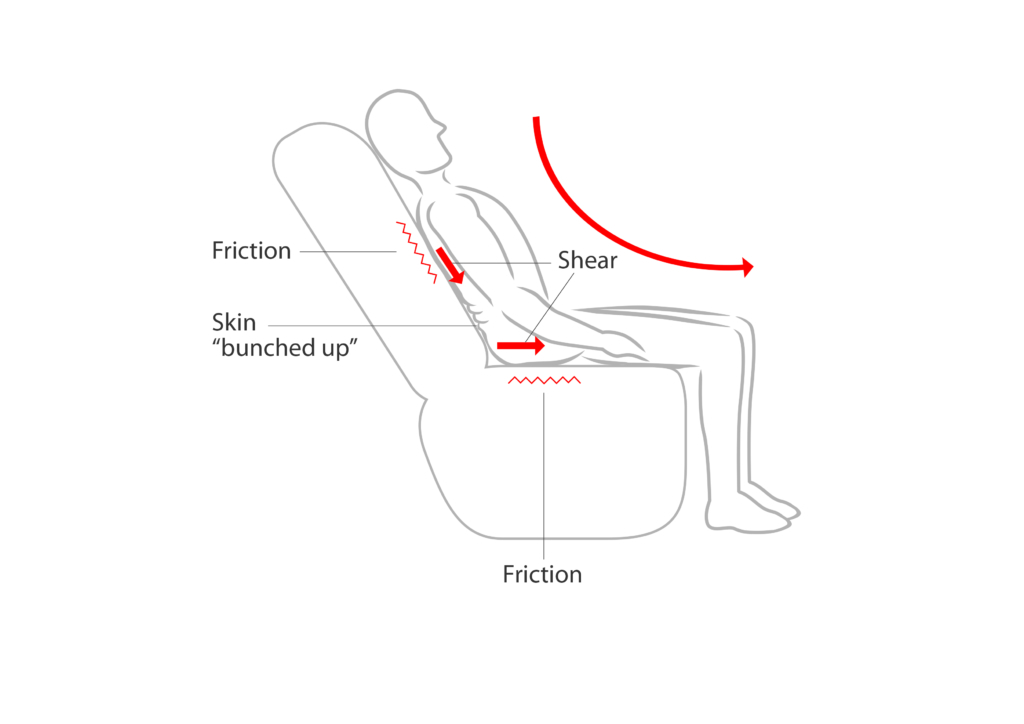
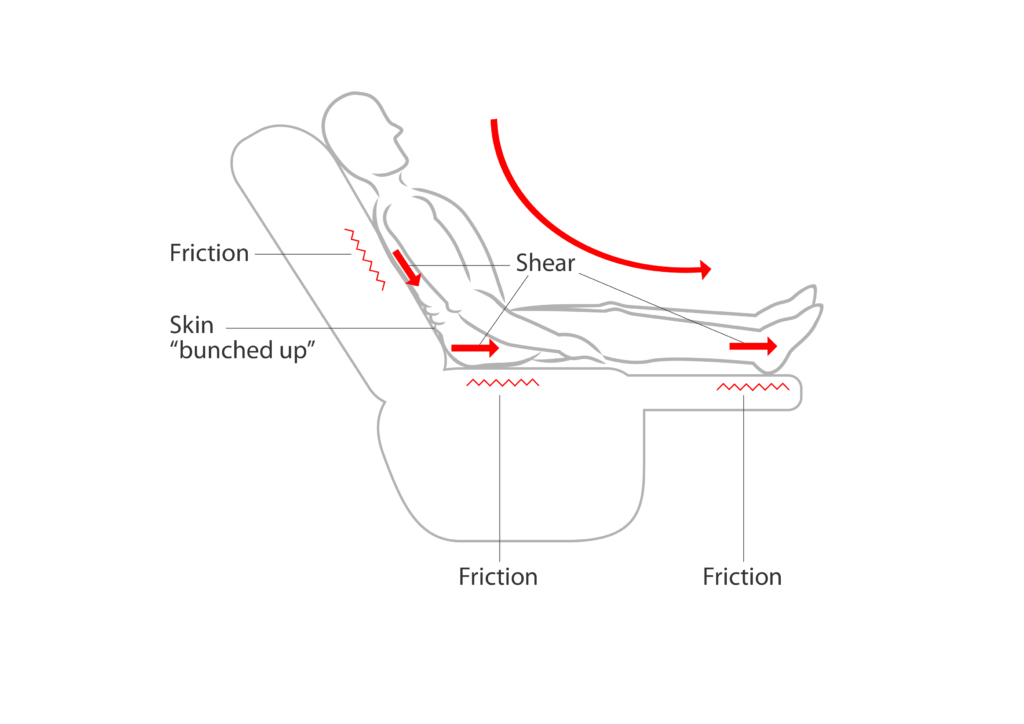
Shear:
If our body moves but the skin that we are sitting on stays still, shear occurs. Slumping or slouching whilst sitting in a chair is a common cause of shear and this can cause internal damage beneath the skin. A poorly fitted or designed chair can encourage slouching in the chair for a client that is unable to maintain a good sitting posture.
We must also remember that assessing for pressure risk is an ongoing process and we should ensure that our clients, their families or care providers are aware of the need for review at any point when the clients risk factors, abilities or care needs change.
Friction:
When the body moves across another surface, such as when our buttocks slides over the surface of a chair, it causes friction. If excessive friction occurs then damage can be caused to our client's skin. We need to carefully consider the moving and handling implications of this and whether friction may be being caused when our client gets in and out of their chair or moves around whilst in the chair.
Considerations when looking for a suitable chair.
When selecting the right chair for our client pressure care is very important. If we are aware of any risk factors they have, along with a knowledge of the way pressure injuries are caused, we can then start to specify the size, features and pressure redistribution qualities of the chair to ensure that it meets the pressure care requirements of our client as part of their larger care and support plan.